By Aubrey Gowing
Like many intriguing stories this one begins with the reveal. The seemingly innocent bicep is thought of primarily as an arm mover. Indeed its role in elbow flexion rather than shoulder flexion is most responsible for biceps calamitous effect on humeral head position; not the most obvious suspect for shoulder impingement. So keep the bicep in the back of your mind as we discuss the other suspects implicated in shoulder pain.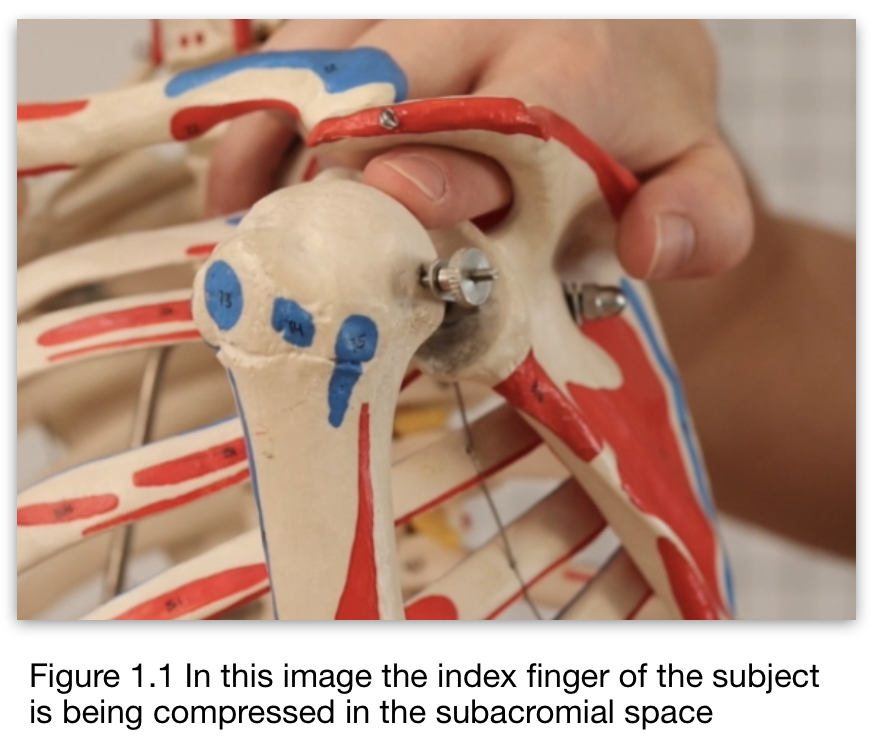
Low back pain, shoulder pain and neck pain are probably the three most common dysfunctions most clinicians deal with. Usually in that order. It’s worth getting to know and thoroughly understand subacromial impingement syndrome (SIS) as it is one of the most common causes of shoulder pain and can cause significant loss of function.[1] Once understood, it is not a difficult condition to treat and a speedy resolution can be achieved.
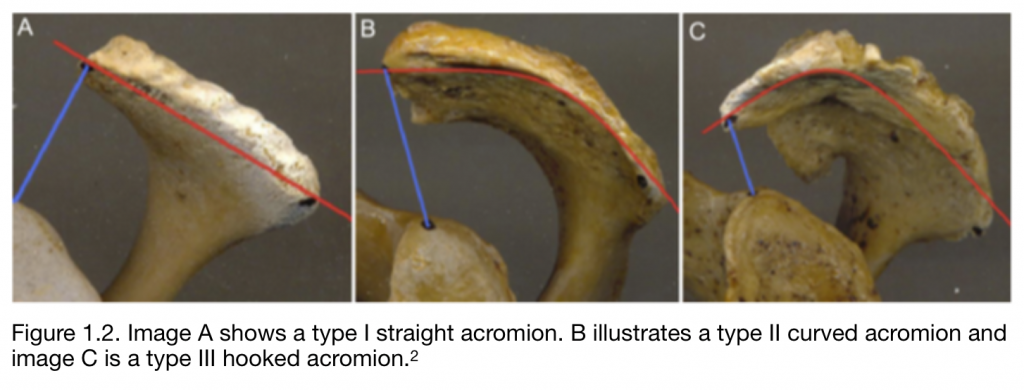
The standard definition of SIS is that the condition is caused by inflammation and irritation of the rotator cuff tendons as they pass through the subacromial space (figure 1.1) resulting in pain, weakness and reduced range of motion within the shoulder complex. In particular abduction and medial rotation are decreased and these movements may provoke a pain response. However supraspinatus and the subacromial bursa are the victims here, not the perpetrators.
(see below video; subacromial impingement part 1)
So what reduces the subacromial space? The three primary contributors are:
- Hooking of the acromion (type III)
- A superior migration of the humeral head
- Poor postural positioning of the scapula
Initial investigation by a medical practitioner will usually involve physical examination and an x-ray to rule out degenerative arthritic changes in the humeral head or congenital hooking of the acromion. Angling or hooking of the acromion is graded from I to III. It is estimated that 43.3% of the population has a type I flat acromion, 47.7% have a type II curved acromion and only 9% have a type III hooked acromion.[2] Some cases of a type III acromion may warrant a surgical intervention (figure 1.2).
With only 9% of the population having a type III acromion, it is not the primary factor responsible for the 65% of anterior-lateral shoulder pain seen in clinic. Once this unlikely culprit has been assessed we can rule it out as a suspect. Range of motion, muscle resistance and orthopaedic testing can narrow the field further.
Testing for impingement
A useful first step in assessing SIS is to have a client actively abduct the arm. Active range of motion tests are comparatively safe as the client performs the movement and they are instructed to stop as soon as discomfort is felt. This avoids irritating the condition with an overly strong provocation test. As soft tissues, osseous tissue and cartilaginous tissues are all in motion, active tests are considered to give general but useful information about the severity of the injury and the nature of the movement that causes discomfort.
This can be followed with passive range of motion tests (figure 1.3). In passive tests, the therapist provides the movement and the client remains relaxed or passive. A passive test provides specific information regarding passive, non-contractile structures e.g. ligaments, joint capsule and articulating cartilage. Additionally we can gather information about true range of motion and end feel.
Finally a muscle-tendon unit can be assessed using a muscle resistance test. Resistance tests are performed by having the client isometrically contract a muscle against resistance, usually provided by the therapist. These tests enable the therapist to differentiate between myofascial pain, neuromuscular pain, and muscle-tendon strain pain. This enables the therapist to accurately locate and treat a strain.
- Myofascial pain will test positive on resistance with the client indicating a diffuse discomfort in the target muscle by moving their finger over the affected area, during the time of the test. Treat with myofascial techniques.
- Neuromuscular pain will test positive but with a pain radiating beyond the target muscle along a recognised referral pattern.
- Muscle-tendon strain will test as a highly localised pain in the target muscle and most commonly at the muscle tendon junction. This painful spot will be small enough to cover with the pad of one finger. Treat with multi-directional friction, pain free movement and progressive eccentric loading until fully resolved.[3]
The most relevant active and passive movements to test for SIS are abduction and medial rotation. As the client abducts their arm observe the quality of the movement, where in the arc of motion the symptoms are felt and where movement is restricted or stops. End feel in passive movement is also important to assess for joint capsule involvement. Supraspinatus can be tested using resisted abduction with the arm held at 20º-30º of abduction.
It’s worth exploring a slight tangent here to discuss the injuries and dysfunctions that can be observed during abduction and what conditions might be indicated. (see below video; subacromial impingement part 2)
0º to 20º If the client experiences pain in the first 0º to 20º of abduction this indicates a supraspinatus tear. Take particular care in a case of recent trauma and refer out for medical attention.
20º to 30º As the client abducts the arm the first condition we may observe is lateral shoulder pain at about 30º of abduction indicating supraspinatus injury. This can be confirmed with a muscle resistance test.
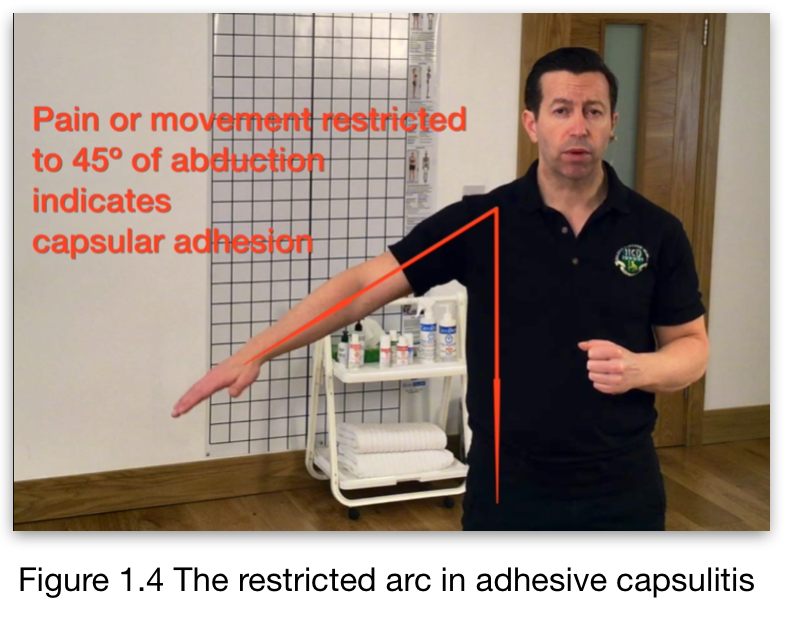
45º At 45º of abduction the restriction caused by adhesive capsulitis will be observed (figure 1.4). There is a tendency for scapular elevation and rotation to be substituted for glenohumeral motion. For an accurate assessment the scapula should be stabilised. The presence of adhesive capsulitis can be confirmed by assessing end feel with a passive test. This will present as a ‘bone on bone like’ end feel.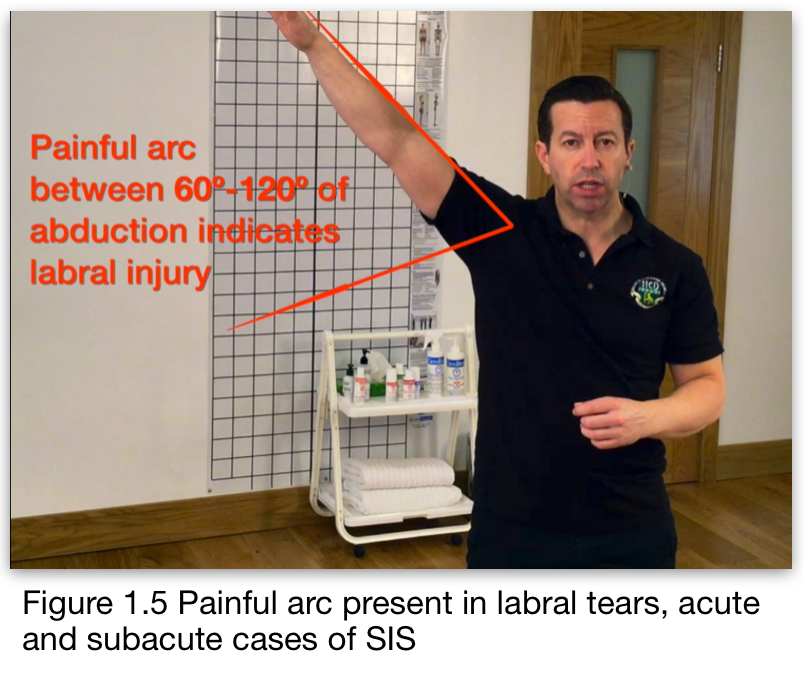
60º to 120º This is referred to as ‘painful arc’ and indicates a possible labral tear and supraspinatus tendon impingement (figure 1.5). This will typically be observed as pain as the humerus drops below shoulder level at about 90º. In the case of a labral tear, a deep clunk may also be felt. Severe cases of SIS may also present in this range and orthopaedic testing will separate out which of these two conditions is present. In cases where the tests seem to conflict, consider that the client may present with both conditions simultaneously.
150º to 175º This will present as restricted range either with or without pain. On a follow up passive test this will present as a springy block or when presenting with some capsular restriction it will test as a ‘bone on bone like’ end feel.
Orthopaedic testing
No one impingement test is ‘the best one’ as tests such as Hawkins, Neer and horizontal adduction test have a high level of sensitivity, while the drop test, painful arc and Yergason test had high specificity values.[4] Speed test has moderate sensitivity and specificity indicating a low clinical value. Combining multiple tests, known as ‘cluster testing’ provides more reliability. All of these tests are aimed at reproducing the client’s recognised pain pattern to confirm the presence of SIS. Referring back to our analogy at the beginning of perpetrator and victim, these tests identify the victim; not the perpetrator.
Performing the tests
Hawkins test. This is a specific subacromial impingement test. The shoulder and elbow of the client are flexed to 90 degrees and then internally rotated with a slight over pressure. The test is positive if it reproduces the client’s recognised pain pattern.[5] This will reliably test as positive when the client has impingement, telling us the condition is present but not identifying the cause.

Neer test. This is also a specific subacromial impingement test. The scapula is stabilised as the client’s arm is internally rotated and brought into forward flexion (figure 1.6), again with a mild over pressure at the end range. The test is positive if it reproduces the client’s recognised pain pattern.[6] This test will identify the bicep as being symptomatic and finally identify our prime suspect!
Horizontal adduction test. This test is useful in assessing acromioclavicular pathology. The arm is flexed to 90º and then horizontally adducted towards the opposite shoulder with the elbow flexed.[7] A mild over pressure is used to push the arm towards the torso. The test is positive if it reproduces the client’s recognised pain pattern.
Drop test. Also referred to as the drop arm sign, this test is used to assess for supraspinatus tendinopathy. The client’s arm is brought into 90º of abduction and externally rotated. The client should be able to control the descent without pain.[8] If the arm drops suddenly and reproduces the client’s recognised pain the test is considered positive for a supraspinatus tear.
Painful arc.
As described earlier, the client moves their arm through abduction and adduction. A recognised pain pattern between 60-120º is considered positive and may indicate a labral tear or supraspinatus tendon impingement.[9]

Yergason test. This test assesses the transverse humeral ligament (figure 1.7) and bicep pathology. The test is performed with the elbow flexed to 90º and the forearm and hand are pronated. The therapist grips the client’s wrist at the distal end of the radius with one hand as the other hand palpates the long head of the bicep tendon as it passes through the bicipital groove. The client then attempts to supinate the hand against the therapist’s resistance. If the tendon is felt to pop out of the groove this indicates a tear in the transverse humeral ligament.[10] If the client’s recognised pain pattern is localised to the bicipital tendon, this suggests injury to the long head of the biceps tendon. Pain felt deep in the shoulder could indicate a SLAP tear.
Speed test. The bicep tendon is assessed for pathology in this test. This test can be performed in two different ways. The original method involves the client starting with the elbow extended and the palm supinated.[9] The arm is then raised to 60º against the therapist’s resistance. As this is a strong provocative test the more common method is to have the client flex the arm to 90º again with the elbow extended and the palm supinated. The client then attempts to hold the arm steady against a downward force applied by the therapist. A positive test will elicit the client’s recognised pain pattern, localised to the bicipital groove.
Many of theses tests are considered to have a low clinical value. Some chronic conditions simply do not have sufficient severity to test positive on anything other than restricted range of motion.
We opened by talking about the bicep and its role in causing shoulder impingement. This can be confirmed by asking the client to extend the arm. In most cases 45º of extension or more will be observed. However, scapulothoracic movement is usually being substituted for true glenohumeral extension. When the scapula is stabilised by the therapist and the same arm extension is performed by the client 0-10º of extension is observed. This indicates an inability of the bicep to fully lengthen. And the restriction is usually found at the distal end of the bicep due to prolonged elbow flexion. This distal end restriction results in the humeral head being driven up in the glenoid fossa when the elbow is extended. This provides final confirmation that bicep is indeed our prime suspect.
Treatment of subacromial impingement.

With the correct perpetrator now clearly identified treatment becomes a simple matter of restoring extensibility to the bicep and centration to the glenohumeral joint. There are several ways to do this and you can include all of your preferred techniques but here is a suggested protocol for achieving this goal. (see below video; subacromial impingement part 3)
Position Client Supine:
- Myofascial technique for anterior deltoid and biceps – Myofascial technique is applied using the palm of the hand, dorsal surface of the fingers and finger pads alternately to work down the front of the upper arm, working from origin to insertion, to address fascial migration in the typically short tight and facilitated anterior deltoid and biceps.(figure 1.8)
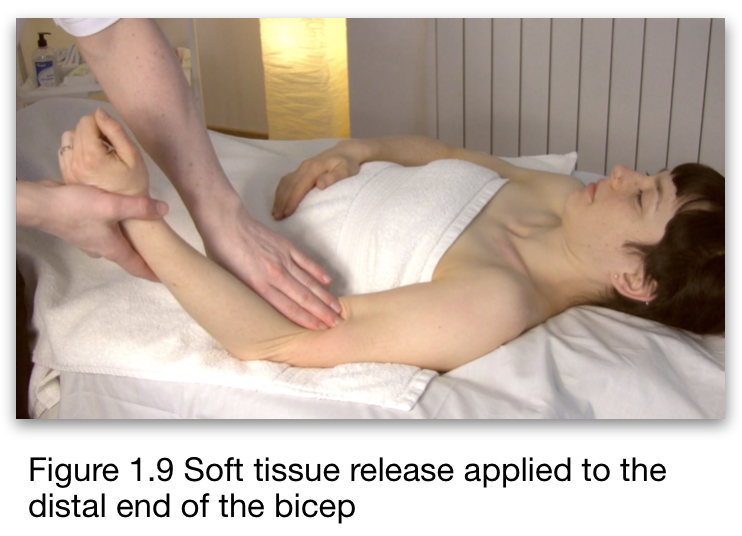
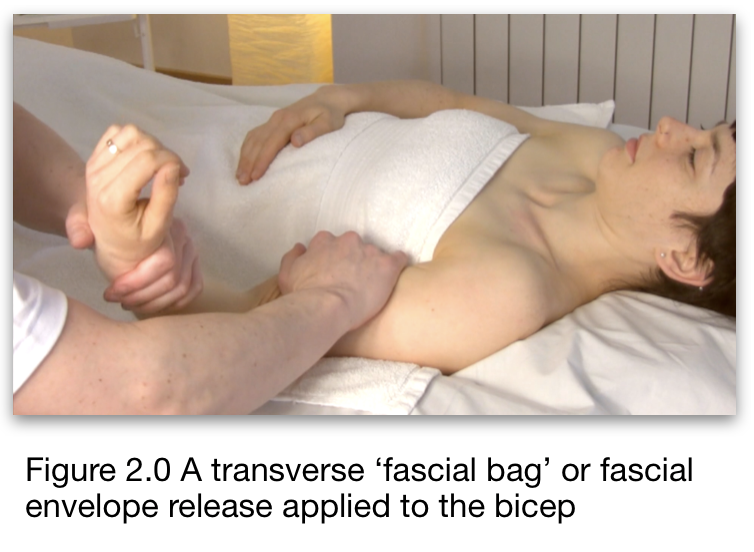
- Soft Tissue Release (STR) and ‘fascial bag’ release for bicep – The elbow is flexed to bring bicep into a shortened position. A lock is then applied with the palm, dorsal surface of the fingers or finger pads, toward the muscle belly as the elbow is extended (figure 1.9). For the fascial bag release the arm is brought into external rotation, the bicep is stretched laterally/externally to pin the muscle, and the humerus is then rotated internally. This can then be applied in the opposite direction. (figure 2.0).
- Soft Tissue Release (STR) and ‘fascial bag’ release for triceps – With the shoulder brought into 90° of flexion soft tissue release can be applied to the triceps. The muscle is shortened by extending the elbow a lock is applied to
 ward the muscle belly and the muscle is lengthened by flexing the elbow. (figure 2.1)
ward the muscle belly and the muscle is lengthened by flexing the elbow. (figure 2.1)
*Optional Neuromuscular technique for triceps
Move the client to a side-lying position: - Webbing Technique to drop humeral head – The client’s elbow is flexed to 90° and the shoulder abducted to 90° the therapist holds the little finger or ulnar border of the client’s hand as the webbed part of the therapist’s other hand holds the humeral head (figure 2.2). The holding hand then rotates and abducts the arm as the hand on the humeral head pushes in an inferior direction (figure 2.3). This technique increases subacromial space and restores joint centration.

Home care for subacromial impingement
Effective home care is also now a simple matter. The regular practise of active isolated stretching will maintain the optimal resting length of the bicep (figure 2.4). A simple belt or strap can be used to decompress the humeral head and maintain joint centration and prevent reoccurrence of subacromial compression.
To stretch the bicep the scapula is first retracted and depressed. Suggest to the client that they ‘try to put the scapula in their back pocket’. The opposite han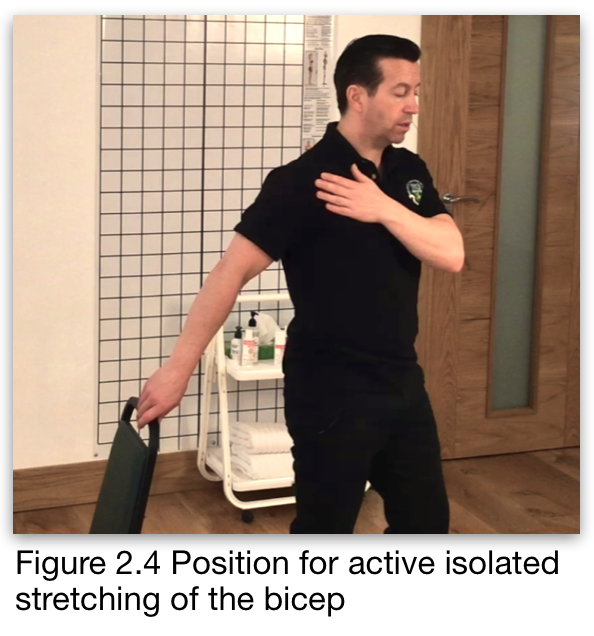 d can be placed on the front of the scapula to monitor the scapula for unwanted protraction or rotation.
d can be placed on the front of the scapula to monitor the scapula for unwanted protraction or rotation.
The client then actively reaches back. The use of a prop like the back of a chair, counter top or table can be used to deepen the stretch provided only very gentle assistance is given. Approximately two or three pounds or about a kilo. Caution the client that excessive force will cause protective muscle contraction that will increase tension instead of the desired effect of reducing muscle tension.
To decompress the humeral head a strap or stretch rope is placed over the proximal end of the humerus. Care must be taken to avoid covering the acromion. The elbow is placed on a soft surface such as the back of an armchair or similar. With the other hand the client pulls down on the strap as they rotate the arm through internal and external rotation. (See video subacromial impingement part 3)
Key takeaway points
- 65% of shoulder pain is caused by subacromial impingement syndrome (SIS)
- Restriction in the distal end of the bicep causes the humeral head to be driven superiorly in the glenoid fossa
- This can cause compression, resulting in possible inflammation and swelling of the tendon of supraspinatus or the subacromial bursa. These are results of misalignment rather than causative factors
- Normalising tissue texture and restoring resting length to the bicep will allow effective mobilisation to drop the humeral head and restore subacromial space.
- Home care exercises can maintain optimal bicep function and humeral head position to prevent reoccurrence.
About the author

Having taught seminars in four continents, Aubrey is a highly regarded international presenter with three decades of clinical experience. He is the current president of the Irish Massage Therapists Association, and author of ‘Myoskeletal and Sports Therapy’. Together with his sister Alison, he co-founded and operates Holistic College Dublin, a successful massage school in their home city of Dublin, Ireland.
Further resources:
References
- Anatomical and biomechanical mechanisms of subacromial impingement syndrome Michener, Lori A. et al. Clinical Biomechanics, Volume 18, Issue 5, 369 – 379
- Aragão JA, Silva LP, Reis FP, dos Santos Menezes CS. Análise da curvatura acromial e sua relação com o espaço subacromial e os tipos de acrômio. Rev Bras Ortop. 2014;49:636–641.
- Clinical Massage Therapy: A Structural Approach to Pain Management. J. Waslaski. Pearson publishing ©2012. ISBN-13: 978-0137063628
- Caliş M, Akgün K, Birtane M, Karacan I, Caliş H, Tüzün F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis. 2000;59(1):44–47. doi:10.1136/ard.59.1.44
- Hawkins RJ, Abrams JS. Impingement syndrome in the absence of rotator cuV tear. Orthop Clin North Am 1987; 18:373–82.
- Neer CS. Anterior acromioplasty for chronic impingement syndrome of shoulder. J Bone Joint Surg 1972;54A:41–50
- Warren RF. Shoulder pain. In: Paget S, Pellicci P, Beary JF, eds. Manuel of Rheumatology and outpatient orthopaedic disorders. Boston: Little, Brown, 1993: 99–109.
- Magee DJ. Shoulder. In: Orthopedic Physical Assessment. Philadelphia: WB Saunders Company, 1992: 90–142.
- Hermann B, Rose DW. Stellenwert von Anamnese und klinischer Untersuchung beim degenerativen Impingement Syndrom im Vergleich zu operativen Befunden-eine prospektive Studie. Z Orthop 1996;134:166–70.
- Yergason RM. Supination sign. J Bone Joint Surg 1931;131: 60.